Anybody who has worked with medical devices knows this truth: just because you’ve submitted the document, it doesn’t guarantee that the work is done. Whether it’s a Clinical Evaluation Report (CER), a Risk Management File, or a Post-Market Surveillance (PMS) Plan, it will be updated, and probably more than once.
And those updates? They rarely arrive when it’s convenient.
A new MDCG guideline drops just days before a submission, a Notified Body returns with clarification questions, or a minor product update now means that the CER needs revalidation. It’s not chaos, it’s just the reality of working under the MDR, where regulations are still settling, the guidance is constantly evolving and updating, and the documentation that is produced is expected to not only reflect current compliance, but also those emerging expectations.
Why It Feels Like Document Writing Never Ends
The concept of ‘final’ documentation doesn’t apply anymore, especially not in this landscape, as the MDR demands living documents. Even well-developed documents are living entities, all subjected to:
- New or updated MDCG guidance
- Shifting interpretations from Notified Bodies
- Internal process changes, product tweaking, or clinical updates
- New PMS or PMCF activity data
- Rolling requirements in the transition from MDD to MDR
Even documents you thought were locked down, like a CER submitted months ago, can be pulled back into circulation because one post-market signal changed the picture. And for those writing under tight timelines and across many products? The challenge isn’t just writing well, it’s writing in a way that stays compliant as the rules shift around you.
How to Stay Sane (and Compliant) When Nothing Stays Still
The good news? While we can’t slow the pace of regulatory change, we can put systems in place to handle it efficiently, reduce repeat effort, and avoid the trap of last-minute document chaos.
Here’s how:
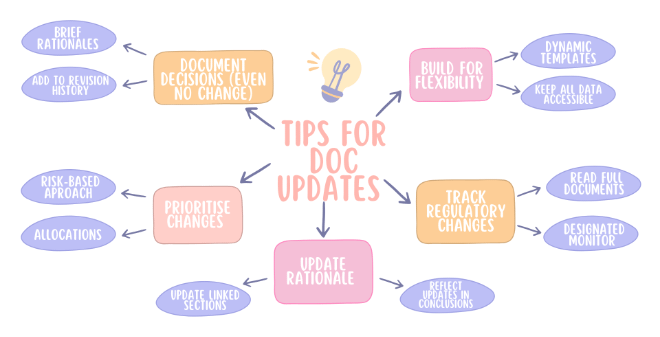
1. Stop Waiting for Stability – Build for Flexibility
If you’re still treating documentation like a one-off event, it’s time to rethink your strategy. Instead, design your processes and even your mindsets around flexibility, not finality.
That means:
- Templates that evolve: Use dynamic templates that include built-in prompts for MDR Article references, GSPRs, and standard alignment. Regularly update these templates as the guidance evolves.
- Accessible source data: Keep literature search strings and extractions, post-market data, and risk management files well-organised and easy to re-source. If you need to update the CER, you shouldn’t have to start a new literature search from scratch.
Tip: Set a regular internal update cycle, quarterly or biannually, even if no immediate updates are required. That way, nothing builds up and you’re never caught off guard.
2. Track (and Interpret) Regulatory Change – Before It Catches You Off Guard
One of the fastest ways to fall out of compliance is to miss a guidance update, or worse, know that one happened but you failed to understand its impact.
To stay ahead:
- Assign responsibility: Designate someone on your team (or a regulatory consultant) to monitor new MDCG, EMA, or ISO publications.
- Create a regulatory watch log: Maintain a simple spreadsheet that includes the date, reference number, a summary of the change, and your internal decision: “has an impact,” “keep monitoring,” or “no action is needed.”
- Don’t rely on automated alerts: Reading the full document and not just the headline makes a difference. Regulatory updates often contain interpretative nuances that affect your documentation indirectly.
Tip: Schedule 30-minute “Reg Change Reviews” on a regular basis. Even a quick discussion of what’s new and who it affects can avoid a fire drill later.
3. Don’t Just Update the Document – Update the Rationale
It’s easy to fall into the trap of tweaking a paragraph or replacing an outdated reference but leaving the underlying justification untouched. That’s where Notified Bodies will notice gaps.
For every update you make, ensure you:
- Revisit the clinical or regulatory rationale behind it and observe what has changed in terms of patient safety, performance claims, or standard expectations.
- Update linked sections: A new literature article may affect the CER, but also the risk management file or IFU. Don’t let your files get out of sync.
- Reflect updates in your clinical conclusions or benefit-risk analysis, as even minor changes can have downstream effects.
Tip: Try writing a “linked document checklist”. If you update the CER, the checklist reminds you to check PMS, Risk, and Labelling too, helping you to avoid siloed changes that don’t tell a coherent story.
4. Know What’s Good Enough – and What Needs Action Now
When everything feels urgent, it’s easy to panic or overcorrect. But not every change requires immediate overhaul.
Use a risk-based approach:
- High priority: Outdated literature reviews, gaps in PMS data, and expired equivalence claims, as these need fast attention.
- Medium priority: Updates to standards or minor inconsistencies in risk files. Make a note of these for the next routine update, or after the high-priority changes.
- Low priority: Editorial updates, visual formatting, or minor changes without performance or safety impact.
This triage approach helps you stay focused and allocate resources effectively, which is a must for all teams.
Tip: How about colour coding in your tracking tools? It makes it easier to visualise what needs immediate attention versus what can wait, especially when reporting to leadership or planning resourcing.
5. Document Your Decision-Making (Even When You Don’t Make a Change)
The MDR is all about transparency and traceability. That applies not only to what you change, but also to what you choose not to change.
Let’s say a new MDCG guideline is released, but after review, you determine it doesn’t apply to your device. You still need to:
- Log the decision with a brief rationale (“Device is non-implantable; MDCG 2023-XX not applicable”).
- Add a line to your Clinical Evaluation or PMS Plan revision history stating, “Reviewed [guidance]; determined no update required.”
Tip: These “no action required” notes are often what prevent requests for clarification from your Notified Body. They show you’ve done your due diligence, even if the result was no change.
Final Thought: You Can’t Control the Changes — But You Can Control How You Handle Them
Yes, updates will keep coming, guidance will evolve, and definitions will tighten. But with the right systems, documentation habits, and mindset, compliance can become sustainable, not just survivable.
Treat regulatory maintenance like a process, not a project. Build responsiveness into your workflows, keep your reasoning clear, and don’t be afraid to seek help when the flood of updates starts to feel like too much.
Overwhelmed? You’re Not Alone.
At Mantra Systems, we help medical device companies turn document chaos into structured compliance. Whether you’re behind on CER updates, navigating new guidance, or just need a better system, we’re here to help you stay ahead without burning out.
Contact us today to discuss how we can support your team.